Receiving a diagnosis for a complex glomerular disease can be overwhelming. Conditions like Focal Segmental Glomerulosclerosis (FSGS), Infantile Nephrotic Syndrome (INS), and Membranous Nephropathy (MN) all target the kidney’s delicate filtering units, leading to the telltale symptom of nephrotic syndrome: excessive protein in the urine. Yet, while they share symptoms, their underlying causes and, consequently, their treatments are vastly different.
At NephCure Inc., we are driven by the urgent need to advance research and provide support for patients navigating these complex journeys. We strive to bring clarity to the science and accelerate the discovery of targeted, effective therapies.
This article provides an in-depth, accessible look at the multifaceted approach to FSGS treatment, clarifies the challenging infantile nephrotic syndrome causes, and details the modern, targeted strategies used for membranous nephropathy management.
Part 1: The Scarring Challenge—FSGS Treatment Strategies
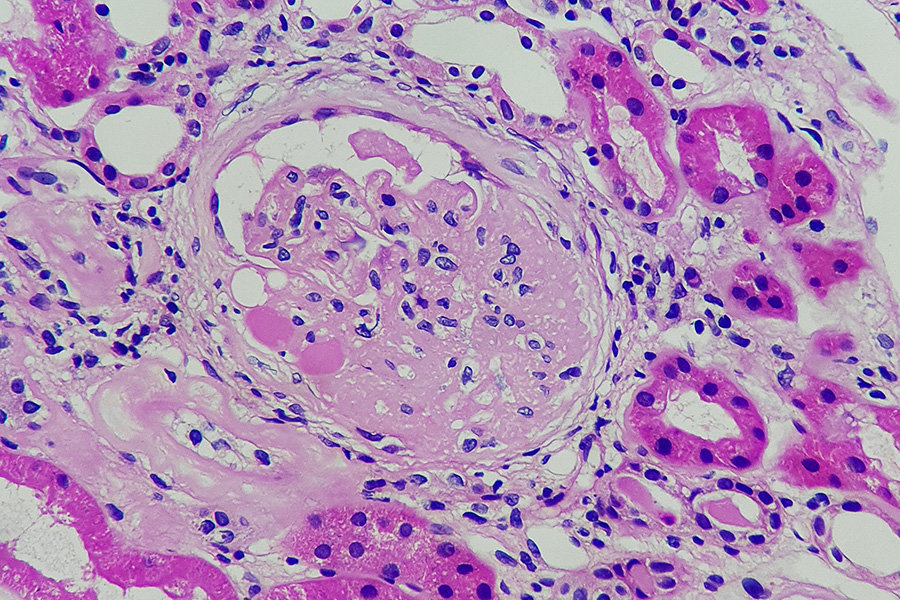
Focal Segmental Glomerulosclerosis (FSGS) is not a single disease but a pattern of injury characterized by scarring in segments of some of the kidney’s filters. It is a leading cause of kidney failure, and effective FSGS treatment requires correctly classifying the disease as primary, secondary, or genetic.
🛡️ Tailoring the Treatment to the Cause
The goal of FSGS treatment is to achieve remission (stopping or severely limiting protein loss) and preserve long-term kidney function.
- Supportive Care (Essential for All FSGS): This is the foundation of management, regardless of the subtype.
- RAS Blockade: Medications like ACE inhibitors or ARBs are critical for reducing proteinuria and controlling high blood pressure, thereby protecting the glomeruli from further damage.
- Lipid and Edema Management: Statins are used to manage high cholesterol, and diuretics help control the swelling (edema) caused by protein loss.
- Immunosuppression (For Primary FSGS): Primary FSGS is thought to be caused by a circulating factor and requires immunosuppression to stop the immune-mediated podocyte damage.
- Corticosteroids: High-dose prednisone is typically the first-line therapy, aiming for remission.
- Calcineurin Inhibitors (CNIs): Cyclosporine or Tacrolimus are the preferred agents for patients who are steroid-resistant or have contraindications to steroids. CNIs are highly effective but require close monitoring to prevent drug toxicity.
- Alternative Agents: Rituximab, Mycophenolate Mofetil (MMF), and high-dose Dexamethasone are considered alternatives, especially for steroid-refractory or CNI-intolerant patients.
- Secondary FSGS: Treatment for secondary FSGS (caused by factors like obesity, hypertension, or certain medications) focuses entirely on addressing the underlying cause and intensifying supportive care. Immunosuppression is generally avoided.
🚀 Hope in Emerging FSGS Therapies
Current research into FSGS treatment is focusing on precision medicine, including:
- Sparsentan: A dual endothelin and angiotensin receptor antagonist that has shown significant promise in reducing proteinuria.
- APOL1 Inhibitors: Targeted therapies in development for individuals with the APOL1 gene variants that increase FSGS risk.
Part 2: Understanding the Origin—Infantile Nephrotic Syndrome Causes
Infantile nephrotic syndrome (INS) refers to the onset of nephrotic syndrome between three and twelve months of age, following the very rare congenital form (birth to 3 months). The majority of infantile nephrotic syndrome causes are genetic, which fundamentally dictates the approach to management.
🧬 The Genetic Blueprint of INS
Unlike the most common form of nephrotic syndrome in children (Minimal Change Disease, which is typically treatable with steroids), INS is overwhelmingly caused by inherited gene defects:
- Monogenic Defects: The most common infantile nephrotic syndrome causes are single-gene mutations affecting the proteins that form the podocyte structure:
- NPHS1 Gene (Nephrin): Mutations in this gene cause the congenital nephrotic syndrome of the Finnish type (the most common cause of CNS), which can also present in the infantile period. Nephrin is crucial for the integrity of the slit diaphragm filter.
- NPHS2 Gene (Podocin): Mutations in this gene cause a steroid-resistant form of nephrotic syndrome that often presents in the infantile or early childhood period.
- *WT1, PLCE1, LAMB2: Less common, but still important, genetic infantile nephrotic syndrome causes that result in structural or functional defects in the glomerular filtering unit.
- Infectious Causes: In rare cases, INS can be associated with congenital infections such as syphilis or toxoplasmosis, which cause immune complex deposition in the kidney.
- Clinical Consequence: Regardless of the specific genetic cause, the common outcome is severe, non-responsive proteinuria that leads to life-threatening complications like severe edema, infection, and blood clots, necessitating intensive supportive care and often, eventual kidney removal and transplantation.
Understanding the specific infantile nephrotic syndrome causes through genetic testing is critical, as the identification of a genetic mutation usually confirms steroid resistance and guides the family toward definitive long-term solutions.
Part 3: The Antibody Attack—Membranous Nephropathy Management
Membranous nephropathy (MN) is the most common cause of nephrotic syndrome in non-diabetic adults. This autoimmune disease is defined by immune complex deposits on the outside of the glomerular basement membrane, causing it to thicken and leak protein. The discovery of the anti-PLA2R antibody has fundamentally changed how we manage membranous nephropathy.
🎯 Targeted and Risk-Stratified Therapy
Modern management of membranous nephropathy is a targeted, risk-stratified approach based on the patient’s level of risk for disease progression, using antibody levels to guide therapy.
- Initial Supportive Care: All patients begin with supportive measures for 6-12 months, as many cases remit spontaneously (go away without strong drugs).
- ACE Inhibitors/ARBs: Used to lower proteinuria.
- Symptom Management: Diuretics for edema and statins for high cholesterol.
- Immunosuppression (For High-Risk Patients): If proteinuria remains high and/or anti-PLA2R antibody levels are elevated, immunosuppressive therapy is initiated to stop the immune attack.
- Rituximab (First Line): This B-cell targeting agent is now a standard, first-line therapy. It reduces the B cells that produce the pathogenic antibodies (anti-PLA2R), leading to immunological remission and a reduction in proteinuria with fewer side effects than traditional chemotherapy.
- Calcineurin Inhibitors (CNIs): Often used in combination with low-dose steroids as an alternative initial therapy.
- Alkylating Agents: Cyclophosphamide, typically used in combination with steroids (e.g., Ponticelli regimen), remains a highly effective option for very high-risk disease, though it carries a greater risk of toxicity.
The key to successful membranous nephropathy management is the integration of antibody monitoring with clinical assessment, allowing clinicians to choose the right therapy at the right time.
The NephCure Inc. Commitment: Your Source for Specialized Knowledge
Whether you are navigating the complex, often individualized FSGS treatment plan, facing the reality of genetic infantile nephrotic syndrome causes, or benefiting from the precision of modern membranous nephropathy therapy, NephCure Inc. is your dedicated partner.
We fund the research that clarifies disease mechanisms and accelerates the development of new drugs, ensuring that the path toward a cure for all glomerular diseases is within reach.
Ready to access resources, learn about clinical trials, and join a supportive community?
Visit the NephCure Inc. website today to find specialized information and support! 📞