IVF treatment involves multiple medications serving different purposes throughout your cycle. Understanding what each medication does, why your doctor prescribed it, and what side effects to expect helps you feel more prepared and less anxious about the pharmaceutical aspect of treatment.
The medication regimen varies significantly between patients based on age, ovarian reserve, diagnosis, and previous response to fertility drugs if you’ve done IUI or other treatments before. Your specific protocol is customized to optimize your response while minimizing risks like ovarian hyperstimulation syndrome.
Ovarian Stimulation Medications
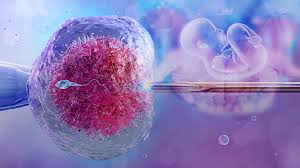
The cornerstone of IVF medication protocols involves injectable hormones that stimulate your ovaries to produce multiple eggs in a single cycle instead of the one egg that typically develops naturally. These medications contain follicle-stimulating hormone (FSH), luteinizing hormone (LH), or combinations of both.
Common stimulation medications:
- Gonal-F or Follistim (recombinant FSH)
- Menopur (combination of FSH and LH)
- Clomid or Letrozole (oral medications sometimes used)
Your doctor determines the starting dose based on your age, AMH levels, antral follicle count, and body weight. Dosing typically ranges from 150-450 IU per day, with adjustments made during monitoring appointments based on how your follicles are responding. Poor responders might need higher doses, while patients at risk for hyperstimulation start with lower doses.
These injections are administered subcutaneously (under the skin) in your abdomen or thigh, usually once or twice daily. The needles are small—much smaller than typical shots—and most patients find them less painful than anticipated. Side effects include bloating, fatigue, mood swings, breast tenderness, and mild abdominal discomfort as your ovaries enlarge with developing follicles.
Ovulation Suppression Medications
While stimulating egg development, you also need medications preventing premature ovulation before egg retrieval. If you ovulate naturally before the retrieval procedure, all those developing follicles release their eggs and the cycle must be canceled.
GnRH antagonists like Cetrotide or Ganirelix are most commonly used for suppression. These daily injections start partway through your stimulation (usually around day 5 or 6) and continue until your trigger shot. They work immediately to prevent the LH surge that causes ovulation.
Alternatively, some protocols use GnRH agonists like Lupron for suppression, which are started before stimulation begins. Long Lupron protocols involve taking Lupron for 1-2 weeks before starting stimulation medications, temporarily shutting down your natural hormone production so the doctor has complete control over your cycle timing.
The choice between antagonist and agonist protocols depends on various factors including your diagnosis, previous cycle responses, and your doctor’s preference based on experience with different approaches.
Trigger Shot for Final Maturation
Once your follicles reach appropriate size (typically 16-20mm in diameter), you’ll receive a “trigger shot” that causes final egg maturation before retrieval. Timing is critical—egg retrieval must occur approximately 35-36 hours after this injection to catch eggs at optimal maturity.
Human chorionic gonadotropin (hCG) triggers like Pregnyl, Novarel, or Ovidrel are most common. Your doctor will give you precise timing—often something like “inject at exactly 10:00 PM tonight” rather than a general timeframe. Set multiple alarms because missing or mistiming this injection can compromise your entire cycle.
Some protocols use Lupron as a trigger instead of hCG, particularly for patients at high risk of ovarian hyperstimulation syndrome. Lupron triggering significantly reduces OHSS risk but requires different post-retrieval protocols.
Post-Retrieval and Transfer Support Medications
After egg retrieval and embryo transfer, you’ll take progesterone supplementation to support the uterine lining and potential early pregnancy. Natural progesterone levels drop after egg retrieval because the puncture of follicles during retrieval disrupts their hormone production.
Progesterone supplementation options:
- Intramuscular injections (most effective but most uncomfortable)
- Vaginal suppositories or inserts
- Oral capsules
- Combination of methods
Progesterone in oil (PIO) injections are thick and can cause significant discomfort, soreness, and bruising at injection sites. These go into your upper buttock muscle and require longer needles than the subcutaneous medications used during stimulation. Many patients dread PIO shots more than any other aspect of IVF medications.
If you achieve pregnancy, progesterone supplementation continues for approximately 8-10 weeks until the placenta takes over hormone production. Some doctors also prescribe estrogen patches or pills during this phase to provide additional uterine lining support.
Additional Medications and Supplements
Beyond the core protocol medications, your doctor might recommend or require additional drugs and supplements based on your specific situation.
Prenatal vitamins should be started at least one month before beginning IVF, with particular attention to folic acid content. Some doctors prescribe CoQ10, vitamin D, DHEA, or other supplements believed to improve egg quality, though scientific evidence for these varies.
Baby aspirin (81mg) is commonly prescribed to improve blood flow to the uterus and reduce clotting risks. Patients with immune issues might take prednisone or other immunosuppressants. Those with thyroid dysfunction need thyroid medication optimization before starting IVF.
Antibiotics are given around egg retrieval to prevent infection, and doxycycline is sometimes prescribed for male partners to potentially improve sperm quality. If you’re doing a medicated frozen embryo transfer cycle, you’ll take estrogen pills or patches for 2-3 weeks before starting progesterone and scheduling transfer.
Managing Medication Costs
The pharmaceutical expenses of IVF often shock patients even when they’ve prepared for the base procedure costs. Medication costs vary dramatically based on your protocol, dosages required, and where you purchase them.
Strategies to reduce medication costs:
- Compare prices at multiple pharmacies
- Ask about discount programs from drug manufacturers
- Check if insurance covers any medications even if they don’t cover IVF
- Consider purchasing from overseas pharmacies (carefully research legitimacy)
- Ask your clinic about medication donation programs
Some clinics maintain medication donation programs where patients who’ve completed treatment donate unused medications to others starting treatment. While you can’t legally resell medications, some clinics facilitate these transfers through official programs.
Buying medications in bulk for multiple cycles sometimes reduces per-cycle costs, though this requires upfront capital and confidence you’ll actually use them. Be cautious with this approach—if your protocol changes or you respond differently than expected, you might have medications you can’t use.
Side Effects and When to Worry
Most IVF medication side effects are uncomfortable but not dangerous. Expect bloating, weight gain from fluid retention, mood swings, headaches, fatigue, and breast tenderness during stimulation. These symptoms intensify as your cycle progresses and your ovaries enlarge with developing follicles.
However, certain symptoms require immediate medical attention. Severe abdominal pain, especially accompanied by nausea and vomiting, could indicate ovarian hyperstimulation syndrome or ovarian torsion (twisting). Sudden weight gain exceeding 5 pounds, difficulty breathing, or decreased urination might signal OHSS.
Warning signs requiring immediate doctor contact:
- Severe abdominal pain or swelling
- Difficulty breathing or chest pain
- Persistent nausea and vomiting
- Decreased urination despite normal fluid intake
- Severe headaches with vision changes
- Heavy vaginal bleeding
Most patients complete their medication protocols without serious complications, but knowing warning signs ensures you seek help promptly if problems develop. Your clinic should provide 24/7 emergency contact information for concerns arising outside business hours.
Injection Teaching and Support
Most fertility clinics provide injection teaching appointments where nurses demonstrate proper medication mixing and injection technique. Attend this session even if you’re comfortable with needles—fertility medications often require specific preparation that differs from pre-filled syringes you might have used before.
Practice with saline or demonstration materials first if possible. Many patients bring partners or support people to injection teaching so they can help with administering medications later. Having someone assist, especially with progesterone injections that go in difficult-to-reach spots, makes the process easier.
Numerous online resources including videos and step-by-step guides supplement what you learn at injection teaching. Patient support groups often share tips about minimizing injection pain, managing side effects, and staying organized with multiple medications taken at different times.
Staying Organized Throughout Your Cycle
Managing multiple medications with different storage requirements, preparation methods, dosing schedules, and administration routes requires careful organization. Create a medication schedule listing what to take when, set phone alarms for injection times, and use a checklist to track each dose.
Store medications properly—some require refrigeration while others should stay at room temperature. Keep syringes, needles, alcohol wipes, and gauze organized in one location. Use a sharps container (available at pharmacies) for safe needle disposal.
Understanding your IVF medications transforms them from frightening unknowns into tools helping you achieve pregnancy. While the pharmaceutical aspect of treatment seems overwhelming initially, most patients quickly develop comfortable routines and find the medications more manageable than they feared before starting.